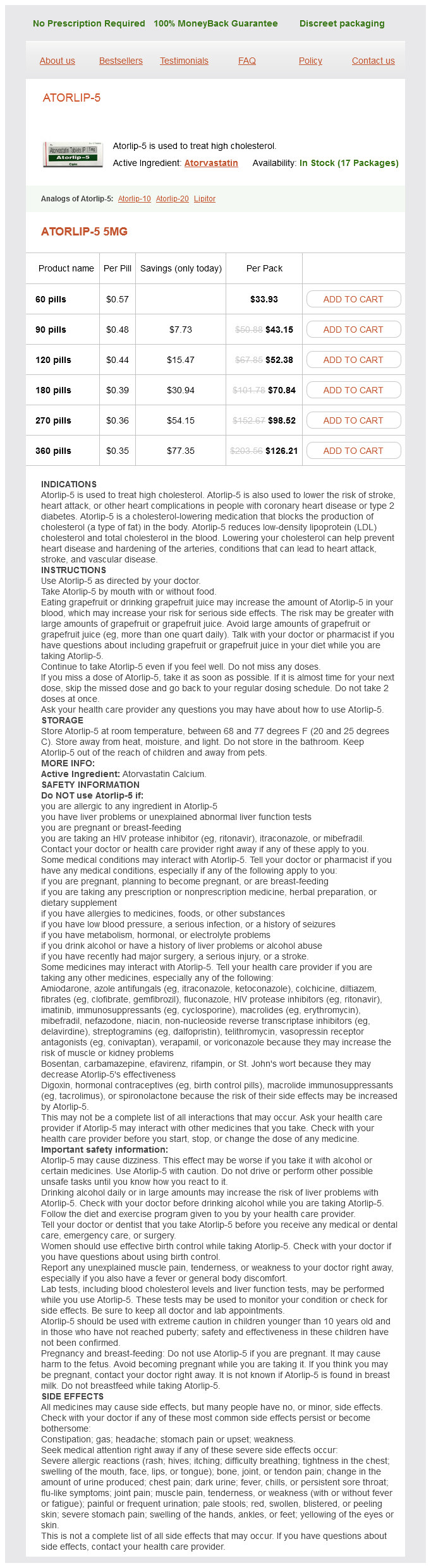
Atorlip-5 5mg
- 60 pills - $33.93
- 90 pills - $43.15
- 120 pills - $52.38
- 180 pills - $70.84
- 270 pills - $98.52
- 360 pills - $126.21
Atorlip-5 dosages: 5 mg
Atorlip-5 packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Only $0.37 per item
In stock: 728
Description
Relative contraindications to laparoscopic repair also include need for prior mesh removal high cholesterol foods to eat list buy atorlip-5 5 mg on-line, presence of an enterocutaneous fistula, and large defects with loss of abdominal wall domain. Recurrence rates and postoperative pain following open or laparoscopic repair seem to be similar, but laparoscopic repair shows lower rates of postoperative wound infections. The intraoperative cost of laparoscopic repair is higher compared to open repair but patients have a shorter hospital stay and thus total costs are similar (B). Approximately one-fourth of the watchful waiting group eventually crossed over to receive surgical repair due to increased hernia-related pain (B). Smaller hernias tend to have a smaller neck, placing them at higher risk for developing incarceration (E). Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. This patient has bilateral inguinal hernias, one of which is recurrent and should be offered a laparoscopic repair. The advantages of this include the ability to visualize both sides through a single incision and a potentially easier surgery in the setting of recurrence. It also protects the patient from developing a femoral hernia since the femoral canal is covered by the mesh. They develop on average sooner than a typical recurrence, suggesting that the original hernia was in fact a femoral one and was missed at the original surgery. Tacking of the mesh in either laparoscopic approach can reduce mesh migration but should be avoided lateral to the epigastric vessels and inferior to the iliopubic tract to avoid placement in the "triangle of doom" or the "triangle of pain," which contain the external iliac vessels and several nerves (lateral femoral cutaneous and femoral branch of genitofemoral, respectively) (B). The preferred initial approach for an uncomplicated inguinal hernia is still actively debated within the surgical community. However, this came at the expense of longer operating room times and higher intraoperative complication rates (B, D). This seems to be consistent with the results of a New England Journal of Medicine study from 2004 comparing open mesh repair to all methods of laparoscopic mesh repair. The most common presentation of a femoral hernia is a painful bulge just inferior to the inguinal ligament, and it is commonly associated with bowel obstruction as well. Though they always enter the groin inferior to the inguinal ligament, it is possible for a part of the hernia to be located above it. Watchful waiting is never indicated, as these hernias are associated with a high incidence of strangulation (1520%) and subsequent bowel ischemia. Open repair can be achieved via a standard suprainguinal incision with a Cooper ligament repair or via an infrainguinal incision directly over the hernia. With this latter approach, a plug of mesh can be rolled into a cigarette shape and used to plug the femoral canal (D).
Syndromes
- Skin cool to touch
- Add coarsely chopped hard cooked egg and cheese cubes to a tossed salad.
- Surgical removal of burned skin (skin debridement)
- Guillain-Barré syndrome
- Breathing support, if needed
- Fatigue
- Good hygiene and routine medical care will help to some degree.
Fissures are tears in the anoderm cholesterol xrd purchase 5 mg atorlip-5 free shipping, and most are superficial and in the posterior midline (poorer blood supply). A deep fissure or one in an unusual location (lateral) should raise concern for Crohn disease. Crohn disease does increase the risk of developing hemorrhoids as well as perianal abscesses and fistulas (CE). Distention of the appendix stretches the surrounding visceral peritoneum and stimulates its afferent fibers, leading to vague and dull periumbilical pain that later transitions to 33. Previously, it was recommended that all patients should undergo surgery after the second episode of uncomplicated diverticulitis. However, several large studies have refuted this, and it is now recommended that surgical intervention be offered on a case-by-basis basis, taking into account the number of episodes, age, comorbidities, severity of attacks, and impact on quality of life. In particular, a lower threshold for surgery is recommended for diabetic and immunocompromised (taking steroids) patients. One of the principles of surgery for diverticulitis is that one only needs to resect inflamed, thickened colon, despite the presence of diffuse diverticula (A, C, E). Once the distal colon is removed, the intraluminal pressure will decrease and the majority of the proximal diverticula will resolve. Recurrence is primarily the result of an inadequate distal resection, which inadvertently may leave behind sigmoid diverticula. Because diverticula do not occur in the rectum, the distal resection margin should be taken at normal-appearing rectum (D). Current indications and role of surgery in the management of sigmoid diverticulitis. Although only a minority of patients (10%) who present with terminal ileitis progress to Crohn disease on longterm follow-up, the surgeon should always consider this diagnosis. The indications for resection would include free perforation, fistula, or stricture. Provided the cecum is not inflamed, the appendix should be removed to avoid confusion in the future because recurrent abdominal pain may develop in the patient. However, in the presence of active inflammation of the cecum, appendectomy should not be performed because there is a higher risk of an enterocutaneous fistula formation (B). Similarly, biopsy should be avoided because this increases the risk for enterocutaneous fistula formation as well (D, E). Therefore, closure of the wound without further intervention is the correct management for this patient. This patient should subsequently receive a colonoscopy with random biopsies to look for evidence of inflammatory bowel disease. Pylephlebitis is essentially an infectious inflammation of the portal venous system.
Specifications/Details
Incision and drainage or percutaneous aspiration are usually not warranted in the absence of a clear area of fluctuance or a fluid collection seen on ultrasound (C) cholesterol in eggs bad for you 5 mg atorlip-5 purchase fast delivery. Mammography is typically not helpful in the workup of mastitis, often resulting in false-positive findings (mass, skin thickening). However, if symptoms and signs of redness and skin thickening persist, mammography and core needle biopsy with or without skin biopsy should be performed to rule out inflammatory breast carcinoma (A, E). The described lesion is a phyllodes tumor, also historically referred to as cystosarcoma phyllodes. These tumors are rare, accounting for fewer than 1% of breast neoplasms, and consist of both an epithelial component and a cellular, spindle cell stromal component that forms a characteristic leaflike structure (hence the term phyllodes). They are predominantly benign, but borderline malignant and malignant variants occur in up to 40% of cases. Phyllodes tumors typically occur in women during the fifth decade of life and commonly present as a fast-growing, firm, mobile mass in the breast. At large sizes, the contours of the tumor are often visible beneath a thin stretched layer of skin, and the size and weight of the tumor cause the breast to take on the shape of a "teardrop. Core needle biopsy is the standard for obtaining a tissue diagnosis, particularly in a woman over 40 years of age. However, benign phyllodes tumors can still be difficult to distinguish from fibroadenoma with core sampling alone, most often being reported as a "fibroepithelial lesion," which require excision in order to make the diagnosis. Distinguishing features of benign phyllodes from fibroadenoma are largely based on stromal hypercellularity and morphology. Recent studies suggest that the best way to distinguish the two lesions is by the proportion of individual long spindle nuclei (>30% is reliable for phyllodes tumors) amid dispersed stromal cells. Excision with a clear margin of breast tissue is the treatment of choice for the vast majority of phyllodes tumors, even malignant ones as long as a margin greater than 1 cm is achievable. For larger, borderline and malignant lesions, mastectomy may be required, but this is not common (E). Borderline malignant and malignant forms of the disease are associated with high local recurrence rates and metastasis via a hematogenous route, most commonly to the lungs. Therefore, sentinel node biopsy and axillary dissection are not indicated, given that phyllodes tumors very rarely metastasize to lymph nodes (C). Radiotherapy is not generally used after lumpectomy (as it is in breast cancer) since phyllodes are most often benign and, even in malig- Breast 139 nant variants, radiotherapy has questionable benefit (D). Chemotherapy has not been proven effective with these tumors and is typically not recommended. Surgical treatment of phyllodes tumors of the breast: retrospective review of 172 cases. Distinction of phyllodes tumor from fibroadenoma: a reappraisal of an old problem.
Linum Usitatissimum (Flaxseed). Atorlip-5.
- Lowering cholesterol levels in people with high cholesterol.
- Are there safety concerns?
- Improving kidney function in people with lupus.
- Osteoporosis.
- Relieving mild menopausal symptoms.
- Dosing considerations for Flaxseed.
- Prostate cancer, diverticulitis, irritable bowel syndrome (IBS), constipation, stomach upset, bladder inflammation, lung cancer, breast cancer, skin irritation, attention deficit-hyperactivity disorder (ADHD), and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96952
Related Products
Usage: q.3h.
Additional information:
Tags: discount 5 mg atorlip-5 mastercard, atorlip-5 5 mg order amex, atorlip-5 5 mg order free shipping, purchase 5 mg atorlip-5 with visa
9 of 10
Votes: 106 votes
Total customer reviews: 106
Customer Reviews
Hamil, 28 years: Acalculous cholecystitis requires urgent intervention, preferably cholecystectomy. Nevertheless, the commonly used therapies usually have broad effects on the overall function of the immune system (Table 15-4).
Osmund, 49 years: Though primary tissue repairs have largely been replaced with tension-free mesh repairs in the treatment of inguinal hernia, they represented a large advancement in reducing recurrence rates of inguinal hernias. The relationship of hypertension and renal failure in scleroderma (progressive systemic sclerosis) to structural and functional abnormalities of the renal cortical circulation.
Achmed, 59 years: Ischemic orchitis is thought to develop as a result of thrombosis of veins of the pampiniform plexus, leading to testicular venous congestion. If a woman desires pregnancy after completing surgery, chemotherapy, and radiation treatments for breast cancer, tamoxifen therapy should be halted to avoid fetal exposure and reinitiated after pregnancy and lactation.
Yugul, 30 years: Although the use of these agents in patients with chronic kidney disease is not contraindicated, they should be used with the consideration that they can cause permanent as well as reversible changes in kidney function. The proximal tubule responds by increasing albumin uptake, most likely via upregulation of the reclamation pathway, thereby minimizing urinary albumin loss.
Malir, 23 years: A physical exam finding is a palpable olive-shaped epigastric mass, although this finding is usually very difficult to elicit. Importance of efferent arteriolar vascular tone in regulation of proximal tubule fluid reabsorption and glomerulotubular balance in the rat.